TAMPA, Fla. (WFLA) — Regeneron and COVID-19 continue to dominate the conversation about how to deal with the pandemic as treatment sites open across Florida.
If you’re not a doctor or medical scientist, you may be asking, “What the heck are monoclonal antibodies?” and “How do they work?”
Here are the answers to some frequently asked questions about monoclonal antibodies.
What are they and what do they do?
Monoclonal antibodies, also called mAbs, are new antibodies made in a lab, according to the U.S. Department of Health and Human Services.
Normally when someone gets sick, their body makes antibodies to fight off the infection. Anyone who’s had a fever or gotten the flu probably knows that sometimes it takes a little time before you get better. That’s because your antibodies have to recognize what type of infection you have, then fight it off.
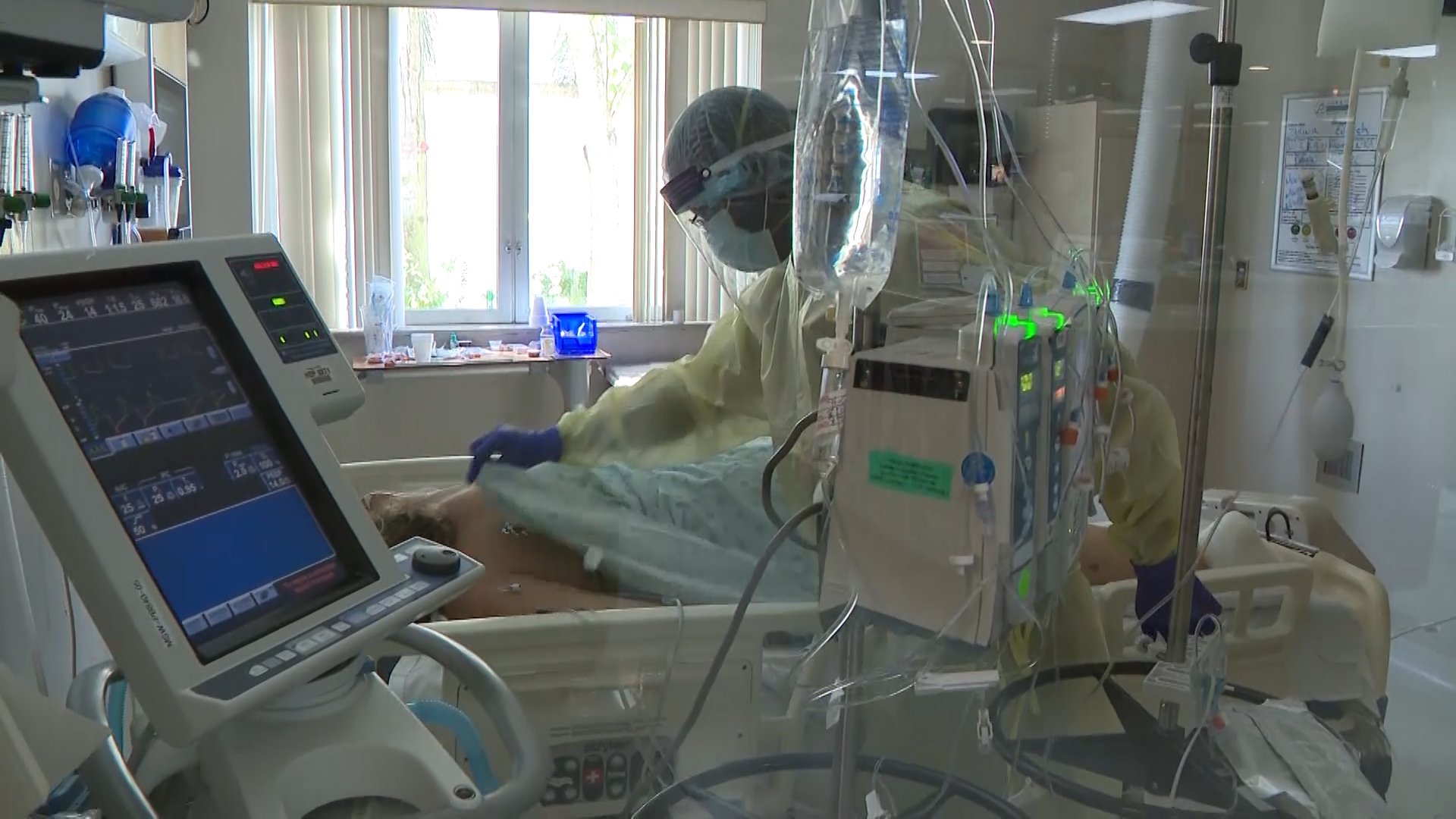
Monoclonal antibodies, like the ones used in Regeneron, and another, similar treatment made by pharmaceutical company Eli Lilly, are made in a lab to target a specific disease. In this case, COVID-19. They’re given to patients who have been infected with COVID, or may have been exposed to it, in order to give them a defense against severe illness, and potentially keep them out of hospitals.
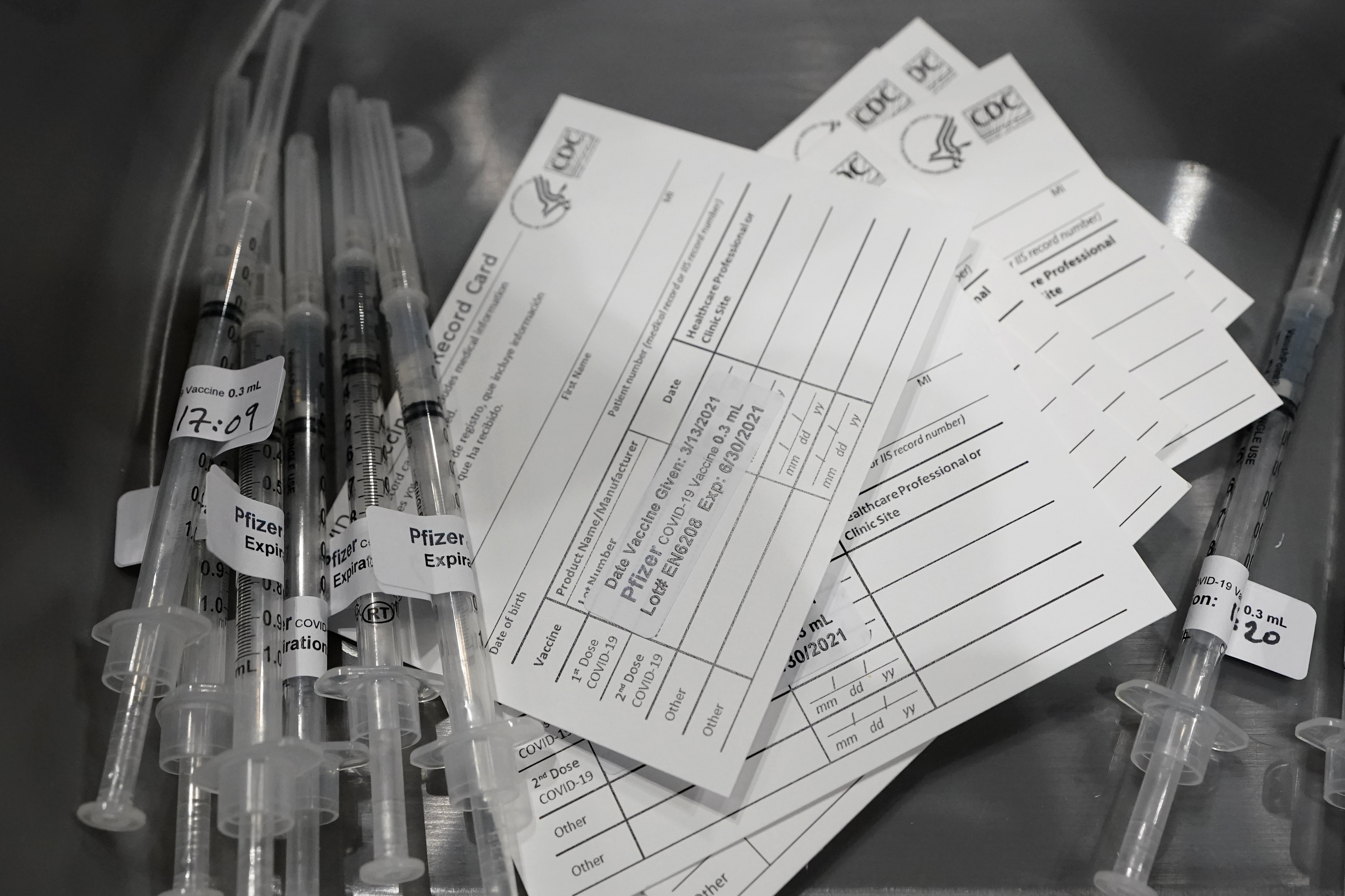
It’s different than the COVID vaccines, but the U.S. Federal Drug Administration approved the mAb treatment around the same time as the shots from Pfizer, Moderna, and Johnson & Johnson were given emergency use authorization. Monoclonal antibodies were approved for emergency treatment by the FDA on June 3, 2021.
mAbs have the same authorization as the vaccines, and just like the shots, the treatment is approved for emergency use for anyone 12-years-old and up. Still, the antibody treatment isn’t a replacement of the vaccine, and it’s recommended to do both.
How do I get it, how do I take it?
In Florida, you have to register to get the treatment, or you can just drive up to a clinic or state-operated site. To get approved to take the treatment, you’ll need to check off a few boxes before you can get it.
First, you’ll need to test positive for COVID-19 within the past 10 days, according to HHS. You’ll also need a referral from a healthcare provider saying you need the treatment. Then you find a place to get the infusion.
Florida has multiple antibody treatment sites springing up across the state. Some are operated by the state government, others are managed by third-parties. There are already a few sites around Tampa Bay, and more are coming.
Once you’re queued up to get the monoclonal antibody treatment, there are two ways to take the therapy.
Usually, it’s taken by IV, an intravenous infusion. Some sites that are providing the treatment may offer an injection instead.
A fact sheet from the FDA, published by Regeneron says that if you’re getting the IV infusion, you can expect a 20 to 50 minute process for the treatment.
Alternatively, if you’re receiving the subcutaneous injection, you’ll be given multiple injections of the treatment, all in separate parts of your body, but around the same time.
If your health care provider determines that you are unable to receive REGENCOV as an intravenous infusion which would lead to a delay in treatment, then as an alternative, REGEN-COV can be given in the form of subcutaneous injections. If you are receiving subcutaneous injections, your dose will be provided as multiple injections given in separate locations around the same time.
Regeneron REGEN-COV fact sheet for monoclonal antibody treatment
Should you get the treatment?
The most important thing to know about the monoclonal antibody treatment is when, or if, you should get it.
The National Institute of Health says the treatment should be used as soon as possible after a patient is diagnosed with a positive case of COVID-19, and within 10 days of symptoms appearing.
The emergency use authorizations for the different monoclonal antibody treatments available include a set of specific conditions that make patients have a higher risk of the virus progressing.
These higher-risk patients included people with conditions like “sickle cell disease, neurodevelopmental disorders, medical-related technological dependence, asthma, cardiovascular disease, hypertension, and chronic lung disease.”
Gov. Ron DeSantis also includes patients with obesity, diabetes, and elderly Floridians as the ones who should consider the Regeneron treatment, especially due to the potential for risk and disease progression.
HHS says not all patients may qualify for the treatment, depending on if they have an underlying health condition that disqualifies you, or if you don’t meet all of the eligibility criteria for the infusions. The agency is encouraging patients not to give up, and says to try to join a clinical trial for COVID-19 as a way to potentially receive the antibodies.
Still, treatment decisions should be considered carefully for benefits and risks to each individual patient by their healthcare providers.